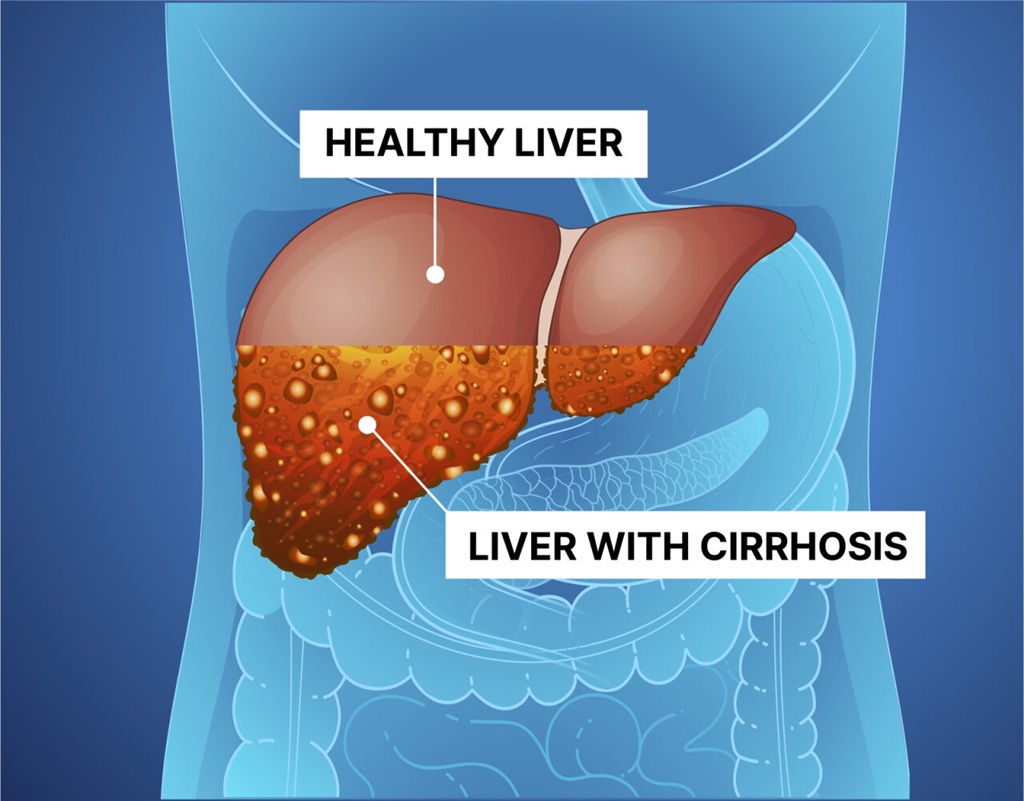
Cirrhosis is a progressive liver disease and a later stage of liver damage. It happens when healthy tissue is replaced with scarred tissue (fibrosis). This scarring affects the liver’s ability to perform its essential functions, including detoxifying the blood, producing bile for digestion, and storing energy. Cirrhosis of the liver is often called a silent condition in its early stages because it can progress significantly before noticeable symptoms arise. This highlights the importance of being aware of the condition and seeking early intervention to prevent further damage.
Understanding liver cirrhosis stages is crucial for recognizing how the disease progresses.
This is the earliest stage, where scarring is minimal, and the liver continues to function effectively. Most individuals at this stage remain asymptomatic, meaning they might not realise they have cirrhosis. However, internal damage has started, and routine health checks or blood tests might reveal abnormal liver enzyme levels. With proper lifestyle changes and treatment of the underlying cause, further progression can often be slowed or halted.
At this stage, liver damage begins to manifest in noticeable symptoms such as mild swelling (edema), persistent fatigue, and occasional digestive discomfort. The risk of complications increases, particularly the development of varices (enlarged veins) in the oesophagus or stomach. These varices may rupture, causing internal bleeding. Early detection and medical intervention are crucial to manage symptoms and prevent further complications.
Severe scarring significantly impairs liver function. Symptoms become more pronounced and include jaundice (yellowing of the skin and eyes), abdominal swelling caused by fluid buildup (ascites), and confusion or forgetfulness due to toxin buildup in the brain (hepatic encephalopathy). The risk of life-threatening complications, such as infections and bleeding, is high. Regular medical supervision and aggressive treatment are often needed to maintain quality of life.
This final stage represents complete liver failure, where the liver can no longer perform its essential functions. Individuals experience debilitating symptoms such as severe jaundice, uncontrollable ascites, and worsening hepatic encephalopathy. At this point, a liver transplant becomes the only viable treatment option. Without a liver transplant, survival rates drop considerably, which is why an early referral to a transplant centre is crucial for improving outcomes.
Identifying signs of cirrhosis early can prevent complications.
The underlying causes of cirrhosis of the liver vary but often involve chronic liver damage.
Diagnosing cirrhosis often involves a combination of physical examination, medical history, and diagnostic tests.
A thorough physical examination can provide initial clues about cirrhosis. Doctors often check for an enlarged liver or spleen, which can signal liver damage. Visible symptoms such as yellowing of the skin and eyes, known as jaundice, may also be observed. These signs suggest the liver’s inability to process bilirubin effectively.
Blood tests are critical for diagnosing cirrhosis of the liver and evaluating its progression. Liver enzyme levels, such as ALT (alanine transaminase) and AST (aspartate transaminase), are measured to detect liver inflammation or damage. Elevated bilirubin levels indicate impaired liver function, while tests for blood clotting time help determine how well the liver is producing clotting factors.
Advanced imaging techniques play a crucial role in assessing liver health. An ultrasound is often the first imaging test conducted to detect liver scarring or abnormalities in liver size. For a more detailed view, doctors may use CT scans or MRIs, which provide a clearer picture of the liver’s structure and any underlying damage.
In some cases, a liver biopsy is required to confirm the extent of damage. This procedure involves taking a small sample of liver tissue for microscopic examination. While invasive, a biopsy provides definitive information about the degree of scarring and helps rule out other liver conditions.
Cirrhosis treatment focuses on slowing the progression of scarring, managing symptoms, and addressing the underlying cause.
If you experience persistent fatigue, swelling, or any of the above-mentioned cirrhosis symptoms, consult a specialist promptly. Residents of Bangalore seeking advanced care can visit their nearest SPARSH Hospital, known as among the best gastroenterology hospitals in Bangalore. We have a team of the best gastroenterologists in Bangalore to help you.
Cirrhosis is a serious condition, but early detection and appropriate management can improve outcomes. Understanding the signs of cirrhosis, its causes, and stages empowers individuals to seek timely medical intervention. If you or a loved one suspects cirrhosis, take action now to safeguard your liver health.
Recovery depends on the stage of cirrhosis. Early-stage cirrhosis may improve with lifestyle changes and treatment. However, advanced stages involving severe scarring are typically irreversible.
Yes, many people with cirrhosis can still live a fairly normal life for many years, even without a liver transplant. This is because the liver is a resilient organ and can keep functioning reasonably well, even if it’s been significantly damaged.
Categories: Gastroenterology
Cirrhosis Of The Liver: Signs & Symptoms, Causes, Stages is available for appointments. Please fill the below form to book an appointment.
Unlock the door to exceptional healthcare, book an appointment with SPARSH Hospital and let your journey to wellness begin.