Introduction
Neutrophils are a crucial component of our immune system, playing a key role in defending our body against infections and other harmful agents. These white blood cells are often the first line of defence against invading pathogens, making them a fundamental part of our innate immune response. Let’s explore what neutrophils are and their functions, normal ranges, and the implications of high or low neutrophil counts.
What are Neutrophils?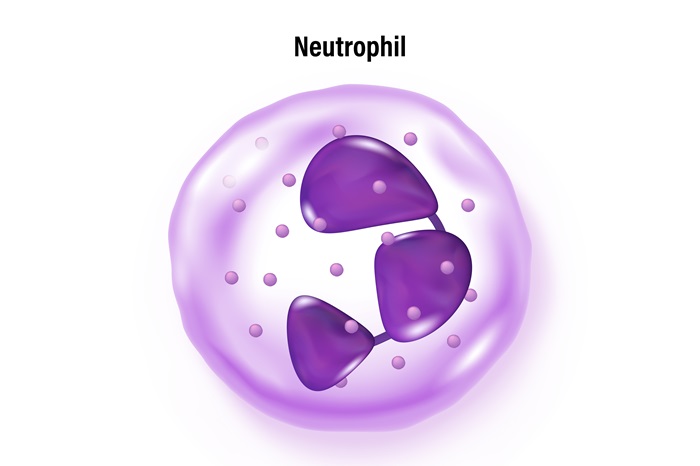
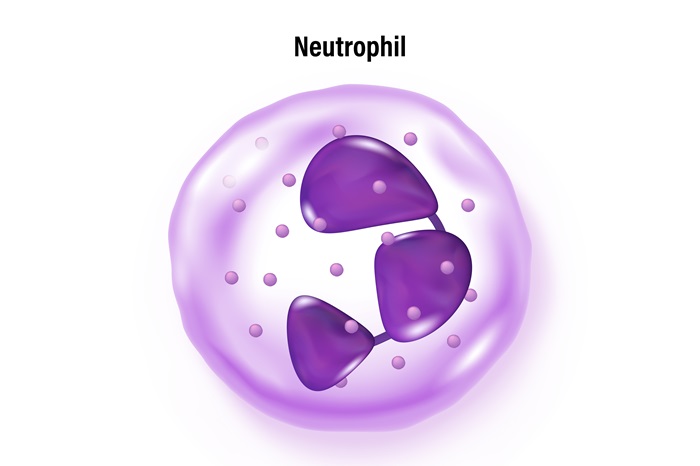
Neutrophils are categorised as white blood cells (leukocytes) that form an integral part of the immune system. They are the most abundant type of white blood cells, accounting for about 40-60% of all white blood cells in the bloodstream. These powerful cells are produced in the bone marrow and have a short lifespan of about 5-90 hours in the bloodstream before migrating into tissues.
These cells are characterised by their multi-lobed nucleus & the presence of granules in their cytoplasm, which contain various enzymes and proteins crucial for their immune functions. The term “neutrophil” comes from their staining characteristics: they appear neutral (neither acidic nor basic) when exposed to certain dyes used in laboratory tests.
Functions of Neutrophils
Neutrophils play several critical roles in the immune system. The following are some common neutrophil functions:
- Phagocytosis: One of the primary functions of neutrophils is phagocytosis, the process of engulfing and destroying foreign particles, bacteria, and other microorganisms. Neutrophils can recognise and ingest these invaders and then use their internal enzymes to break them down.
- Release of Antimicrobial Substances: Neutrophils contain granules filled with various antimicrobial proteins and enzymes. When activated, they can release these substances to kill pathogens extracellularly.
- Development of Neutrophil Extracellular Traps (NETs): In certain situations, neutrophils can release their DNA and associated proteins to form web-like structures called NETs. These traps can ensnare and kill pathogens, preventing their spread.
- Inflammation Regulation: Neutrophils play a role in initiating and regulating the inflammatory response. They release signalling molecules called cytokines & chemokines that bring other immune cells to the infection or injury site.
- Wound Healing: After the initial inflammatory phase, neutrophils contribute to wound healing by clearing debris and promoting tissue repair.
Common Conditions that Affect Neutrophils
Several conditions can affect neutrophil counts and function:
- Infections: Bacterial, viral, or fungal infections often cause high neutrophil count as the body fights off the pathogens.
- Autoimmune Disorders: Lupus or rheumatoid arthritis (RA) can affect neutrophil function and count.
- Bone Marrow Disorders: Leukaemia, aplastic anaemia or other bone marrow conditions can impact neutrophil production.
- Medications: Certain drugs, including chemotherapy agents, can suppress neutrophil production or function.
- Chronic Inflammatory Conditions: Diseases like inflammatory bowel disease can lead to altered neutrophil counts.
- Genetic Disorders: Some inherited conditions can cause impaired neutrophil function or production.
Neutrophilia Causes
A high neutrophil count, also known as neutrophilia, can be caused by various factors:
- Bacterial Infections: The most common cause of neutrophilia.
- Inflammation: Chronic inflammatory conditions can lead to persistently elevated neutrophil counts.
- Stress: Physical or emotional stress can temporarily increase neutrophil levels.
- Medications: Corticosteroids and certain other drugs can cause neutrophilia.
- Smoking: Chronic smoking can lead to increased neutrophil counts.
- Cancer: Some types of cancer, particularly leukaemia, can cause neutrophilia.
- Pregnancy: Neutrophil counts naturally increase during pregnancy.
Causes of a Low Neutrophil Count
A low neutrophil count, known as neutropenia, can be caused by:
- Viral Infections: Some viruses can temporarily suppress neutrophil production.
- Autoimmune Disorders: When the immune system attacks neutrophils.
- Bone Marrow Disorders: Diseases affecting the bone marrow’s ability to produce neutrophils.
- Chemotherapy: Many cancer treatments can suppress neutrophil production.
- Severe Infections: In some cases, severe infections can deplete neutrophil reserves.
- Nutritional Deficiencies: Severe vitamin B12 or folate deficiency can affect neutrophil production.
- Genetic Disorders: Some inherited conditions can cause chronic neutropenia.
Normal Range for a Neutrophil Count
The neutrophil’s normal range can vary slightly between laboratories, but generally:
- For adults: 1,500 to 8,000 neutrophils per microlitre of blood
- For children: The range can be wider and varies with age
Tests to Check the Health of Neutrophils
Several tests can assess neutrophil health and function, such as:
- Complete Blood Count (CBC): This common blood test measures the blood levels of different blood cells, including neutrophils.
- Differential White Blood Cell Count: It gives a more detailed breakdown of the different types of white blood cells, including the percentage and absolute number of neutrophils.
- Bone Marrow Biopsy: Sometimes, a sample of bone marrow may be examined to assess neutrophil production.
- Neutrophil Function Tests: These specialised tests can assess how well neutrophils are performing their various functions, such as phagocytosis.
- Genetic Testing: Doctors may conduct genetic tests for suspected inherited neutrophil disorders.
Treatments for Neutrophil Conditions
Treatment for neutrophil-related conditions depends on the underlying cause:
For Infections: Antibiotics or other antimicrobial treatments may be prescribed.
For Neutropenia:
- Granulocyte colony-stimulating factor (G-CSF) may be used to stimulate neutrophil production.
- In severe cases, neutrophil transfusions might be necessary.
For Neutrophilia:
- Treatment addresses the underlying cause, such as treating an infection or inflammatory condition.
For Autoimmune Disorders: Immunosuppressive medications may be used to prevent the immune system from attacking neutrophils.
For Genetic Disorders: Treatment is typically supportive and may include preventive antibiotics and G-CSF.
Lifestyle Modifications: In some cases, changes in diet, exercise, or stress management may help support healthy neutrophil function.
Conclusion
Neutrophils are a critical component of our immune system, serving as the first line of defence against many pathogens. Understanding their function, normal ranges and the implications of abnormal neutrophil counts is crucial for maintaining overall health. While variations in neutrophil counts can be indicative of various health conditions, it’s important to remember that these numbers should always be interpreted in the context of an individual’s overall health status and other clinical findings.
Regular health check-ups, including neutrophil blood tests, can help monitor neutrophil levels and overall immune function. If you have concerns about your neutrophil count or immune health, it’s always best to consult a doctor for personalised advice and treatment.
Frequently Ask Questions
What happens if neutrophils are high?
High neutrophil counts, or neutrophilia, often indicate that the body is fighting an infection, typically bacterial. It can also be a sign of inflammation, stress, or certain medications. In some cases, persistently high neutrophil counts may suggest more serious conditions like leukaemia or other blood disorders.
What is the function of neutrophils?
Neutrophils have several crucial functions in the immune system:
- Destroy harmful microorganisms
- Regulation of inflammation
- Contribution to wound healing processes
These functions make neutrophils vital to the body’s innate immune response.
What does it mean if your neutrophils are low?
Low neutrophil counts, or neutropenia, can indicate several conditions:
- Viral infections
- Bone marrow disorders
- Autoimmune disorders
- Side effects of certain medications, particularly chemotherapy drugs.
- Severe bacterial infections
- Some genetic disorders
What are neutrophils known for?
Neutrophils are best known for:
- Being the most abundant type of white blood cell in the blood.
- Acting as the body’s first line of defence against infections, particularly bacterial infections.
- Their ability to quickly respond to and neutralise threats through phagocytosis and the release of antimicrobial substances
- Their role in initiating and regulating inflammation
- Their distinctive appearance under a microscope, with a multi-lobed nucleus and granules in the cytoplasm.
- Their short lifespan and rapid turnover in the body
These characteristics make neutrophils crucial players in the innate immune system, providing immediate protection against many pathogens.