The liver is the body's largest internal organ, responsible for crucial functions like filtering toxins, producing bile, and storing energy. However, certain conditions can disrupt its normal functioning. One of the most common is fatty liver disease, where fat builds up in the liver, potentially leading to inflammation, scarring, and, in severe cases, liver failure.
This guide will provide a comprehensive overview of fatty liver, including its causes, symptoms, diagnosis, and treatment options.
Fatty liver is a condition in which excessive fat accumulates in the liver cells. While some individuals experience no symptoms, others may develop fatigue, abdominal pain, or liver dysfunction. Diagnosis typically involves blood tests and imaging, and treatment focuses on lifestyle changes, weight loss, and, in some cases, medications.

Fatty liver disease is the buildup of excess fat in liver cells. Normally, the liver contains a small amount of fat, but when fat exceeds 5% of the liver's weight, it is considered abnormal. This condition can be classified into two major types:
Non-alcoholic Fatty Liver Disease (NAFLD) This form occurs in individuals who consume little to no alcohol. It is associated with obesity, diabetes, high cholesterol, and metabolic syndrome. NAFLD can lead to a more severe condition called non-alcoholic steatohepatitis (NASH). NASH is identified by inflammation in the liver, which can increase the chances of developing more serious complications like cirrhosis or liver cancer.
Alcoholic Fatty Liver Disease (AFLD) Alcoholic fatty liver disease is the result of too much alcohol is consumed over time. The liver processes alcohol, but drinking too much can overload the liver, causing fat to build up and leading to liver damage.
Alcoholic fatty liver disease is the result of too much alcohol is consumed over time. The liver processes alcohol, but drinking too much can overload the liver, causing fat to build up and leading to liver damage.
Fat accumulates in the liver when the balance between fat production and fat removal is disrupted. Key factors include:
One of the challenges of fatty liver disease is its silent progression. In its early stages, many people are asymptomatic. However, as the condition advances, symptoms may include:
Fatigue and Weakness: A general feeling of tiredness and low energy.
Abdominal Discomfort: Pain or fullness in the upper right side of the abdomen, often referred to as fatty liver pain.
Swelling (Edema): Fluid accumulation in the legs or abdomen.
Jaundice: Yellowing of the skin and eyes in severe cases.
Fatty liver disease can affect both men and women, but there may be some differences in how the symptoms show up based on gender.
Fatty liver disease progresses in five distinct stages, each reflecting the severity of liver damage. Early intervention and proper management can prevent further complications and help improve the condition.
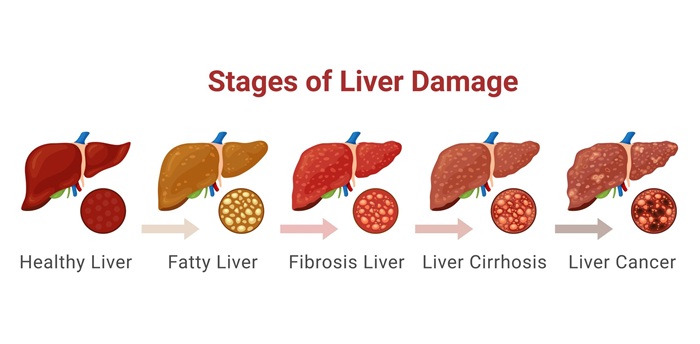
This is the earliest stage, where excess fat accumulates in the liver cells without causing permanent damage.
If inflammation continues, it causes scarring (fibrosis) in the liver. This stage indicates ongoing liver damage, but the liver can still perform some functions.
Cirrhosis represents more severe liver damage, where the liver is heavily scarred and its ability to function is significantly impaired.
Liver cancer can develop as a result of prolonged liver damage, particularly in individuals with cirrhosis or chronic inflammation.
Liver failure is the final, most severe stage, where the liver can no longer perform its essential functions, such as detoxification, protein synthesis, and bile production.
Understanding the causes of fatty liver disease helps identify individuals at risk.
Factors contributing to NAFLD include:
Conditions like acute fatty liver in pregnancy (AFLP) are rare but serious, requiring immediate medical attention. It occurs in about 5 out of every 100,000 pregnancies.
Key causes include:
Key causes include:
Detecting fatty liver disease often requires a combination of tests and procedures:
Managing fatty liver disease focuses on addressing underlying causes and preventing progression.
Weight Loss: Gradual weight loss of 7–10% can significantly improve liver health.
Healthy Diet: A Mediterranean diet, rich in whole grains, fruits, vegetables, and lean proteins, is recommended. Avoid processed foods and high-sugar items.
Regular Exercise: Aim for at least 150 minutes of moderate exercise weekly.
While no specific fatty liver disease medication is approved, treatments target associated conditions:
Diabetes Management: Insulin-sensitizing agents help reduce liver fat.
Lipid-Lowering Drugs: Statins may be used to control cholesterol levels.
Emerging Therapies: Research is underway to develop targeted treatments for non-alcoholic fatty liver disease.
For AFLD, complete cessation of alcohol consumption is critical to halt progression.
Preventing fatty liver involves maintaining a healthy lifestyle:
Book an appointment with a hepatologist if you experience symptoms like persistent fatigue, severe abdominal pain, or jaundice. Regular check-ups can help detect and manage fatty liver disease early.
Fatty liver disease is a manageable condition, but early detection is crucial to prevent complications. Adopting a healthier lifestyle, addressing underlying conditions, and following your doctor’s advice are essential steps. If you're experiencing symptoms or are at risk, schedule a consultation with your healthcare provider.
What Are the Signs of Fatty Liver Problems?
The signs of fatty liver problems may not always be noticeable, especially in the early stages, but as the condition progresses, certain symptoms can appear, such as:
It is essential to pay attention to these symptoms and consult a healthcare provider if they appear, as they could indicate a progression of liver damage.
Can Fatty Liver Be Reversed?
Yes, in many cases, fatty liver can be reversed, especially if it is detected in its early stages. The liver is a remarkable organ with the ability to heal itself under the right conditions. To reverse fatty liver, consider:
Lifestyle changes play a critical role in reversing non-alcoholic fatty liver disease (NAFLD) and improving overall health.
Can I Live a Normal Life with a Fatty Liver?
Yes, it is possible to live a normal life with a fatty liver condition, provided you take proactive steps to manage it. This requires: